Stendra
Discount stendra express
Nuclear stratifcation 234 Turk J Gastroenterol 2014; 25: 233-47 Kayacetin and Guresci treatment xanax withdrawal generic 100mg stendra. Lamina propria expanded with infammation Lamina propria with little or no infammation Acute Gastritis Erosion, edema, hemorrhage Caustic injury, Alcohol Shock, hypotension Difuse Focal Granuloma(s) latrogenic: Iron, etc. Barry Marshall and Robin Warren, who with tenacity and a prepared mind, challenged pre vailing dogmas By using technologies generally available Helicobacter pylori can hold any part of the gastric mucosa, but it most frequently settles in the antrum and cardia, and it often advances to the fundus with treatment. The infammation process is followed by erosion, ulceration, Difculty in implementation and artifacts. Atrophy of the gastric mucosa makes the mucosa thin and thereby causes severe mucosal injury. The As a result of the destruction of glands along with mucosa or densest surface should be assessed. After the atrophy develops, intestinal Helicobacter pylori, the dominant factor in gastritis etiology, was metaplasia replaces gastric mucosa. In 1939, Doenges showed spiro Changes in surface epithelium chetes in the stomachs of 43% of 242 autopsies. Fung identifed a spirochete in the curves of surface mucus cells in chronic gastritis, and in 1983, Warren and Marshall showedthe diferences from artifact separation are fbrin, neutrophils. Foveolar hyperplasia Then, plenty of bacteria, which showed similar growth to gram Increase in length and curving of foveola. Robin Warren (Pathologist) Pancreatic acinar metaplasia Barry Marshall (Gastroenterologist) Lobules that resemble pancreatic acinus 237 Kayacetin and Guresci. Turk J Gastroenterol 2014; 25: 233-47 In autoimmune gastritis In cardia Along with other metaplasia In intestinal metaplasia focus in antrum Thin granulose and acidophilic in apical Basophilic in basal. Superfcial gastritis Band-shaped in superfcial mucosa However, it may not disappear months or years after eradica Lymphocyte, infltration of plasma cells tion. Vacuolar changes foveola in gland epithelium, acidophil, protrusions like clout nails to wards lumen, hyperplasia in smooth muscle fbers in antrum, Severe: Mucosal erosions and glandular microabscess 3). Chronic infammatory re sponse is limited to superfcial mucosa in the beginning 2. Updated Sydney Classifcation Feature Definition Gradind Guidelines Chronic Increased lymphocytes and plasma Mild, moderate, or severe increase in density infammation cells in the lamina propria Activity Neutrophilic infltrates of the lamina Less than one third of pits and surface infltrated = mild; one third to propria, pits, or surface epithelium two thirds = moderate; more than two thirds = severe Atrophy Loss of specialized glands from either Mild, moderate, or severe loss antrum or corpus Intestinal Intestinal metaplasia of Less than one third of mucosa involved = mild; one third to two thirds = metaplasia the epithelium moderate; more than two thirds = severe. The biopsies should be tagged and sent in three separate Lymphocytic gastritis if this increases The biopsy sample that will be taken in the full layer from done far from lymphoid follicles (8). If there is atrophy both with thologists, especially about atrophy, atrophy and intestinal meta and without metaplasia in the same biopsy, it is a better ap plasia were reviewed again. Two main phenotypes of chronic proach to evaluate the atrophy with metaplasia, since the gastritis in the new description of atrophy were classifed as: metaplasia increases the risk of cancer. If the metaplasia is limited to the foveolar epithelium and has not replaced the gastric glands completely, atrophy Updated Sydney Classifcation (Table 1). In this case, the lesion may be de scribed with a metaplasia that is limited to the foveolar Points to take into account while making the Sydney clas focal or partial metaplasia. While atrophy without metaplasia is being evaluated, the and one from the incisura angularis, fve biopsies should be number of glands in x40 enlargement should be taken as 239 Kayacetin and Guresci. In this case, a di Non-atrophic gastritis agnosis of atrophy can be made only with the endoscopic Sydney fndings. Since the lesion Pangastritis (or corpus dominant/predominant non-atro is often patch-like, it is important to identify the location of phic gastritis) biopsy (11). The risk of multifocal atrophic gastritis, metaplasia, and cancer Complete: Goblet cells that contain acidic mucin and absorp is high. Corpus dominant (limited to corpus/corpus predominant) Incomplete: Irregularly shaped goblet cells and immature atrophic gastritis intermediary mucus cellsthe risk of cancer has increased in these cases. This kind of metaplasia should also be accepted set, appropriate tagging, and endoscopic report. Even in benign lesion diagnosis, biopsies should be taken from the right place, with the sufcient amount. For instance, since the microorganisms may be dispersed in a patch man ner in Helicobacter pylori gastritis, Helicobacter pylori may be negative if multiple samples are not taken from diferent localizations. Similarly, if the biopsy is taken from the middle and surface of an ulcerous lesion, a carcinoma that causes Figure 4. Nuclear hiperkromazi, nucleus/stoplazma percent increase seen ulceration underneath or a lymphoma infltration cannot be in the regenerative atypia. Technically, another important problem is the mechanical artifact that is made by the biopsy forceps. When the benign Why is there an apparent atrophic background in some can nature glands get squeezed and lose their normal shape as a cers while there is none in others Since the cell nuclei in the artifacts, which are at the margin of the Infammation pattern risk of cancer. The mononuclear cells that are in the normal limits in the mucosa may appear to be Every step of the cascade. More apparent in societies where in great numbers as a result of contusion artifacts and thus be the risk of gastric cancer is high! But, its rela Another condition for a correct diagnosis is an examination tionship with gastric cardia Despite some other problems that are faced in the evaluation Correa pathway / Correa cascade of benign lesions in endoscopic biopsies, the main problem is Chronic gastritis the diferential diagnosis of whether the lesion is neoplastic or Atrophic gastritis 241 Kayacetin and Guresci. Turk J Gastroenterol 2014; 25: 233-47 Intestinal metaplasia as presence of abnormal mitosis, back-to-back gland pattern, Dysplasia and budding, and papillary formation (13). Gastric cancer In endoscopic biopsies, after diagnosing dysplasia, the second In lesions that are formed by Helicobacter pylori or non-ste crucial point is the distinction of high-and low-grade dysplasia, roidal anti-infammatory drugs (gastritis, ulcer/adjacent to ero and especially in an intramucosal carcinoma diagnosis, various sion) and especially in the intestinal metaplasia zone, it could histopathological approaches among pathologists is a much be difcult to diferentiate regenerative changes from low debated issue. Although an apparent invasion is not seen in most of the Besides the fact that ulcer/erosion adjacency or intense active high-grade dysplastic lesions, Japanese pathologists evaluate infammation is mostly considered to be in favor of regenera it as intramucosal carcinoma (15). While Japanese pathologists tion, it should not be forgotten that active infammation can evaluate only in accordance with the degree of cytologic and also be observed in low-grade dysplasia. The regenerative structural atypia, the incidence of lamina propria invasion is an changes being limited to the glands proliferative zone and not indispensable criterion in the West (16-18). In order to prevent advancing to the surface epithelium and absence of structural this diference and to make the whole world use the same ter deformation are useful for diagnosis. Foveolar hyperproliferation (seen with erosion or ulcer, no intestinal metaplasia) Diagnosis according to Japanese pathologists: Intramucosal Carcinoma 2. Hyperproliferative intestinal metaplasia (back-to-back gland pattern, consists of medium/high number of intestinal In the grading of dysplasia, the triplet system (low-, medium-, glands with mitotic character). In general, it shows that the cells many centers in the form of a doublet grading system, which proliferative activities, such as hyperbasophilia, nuclear and was dysplasia-negative, indefnite group for dysplasia and nucleolar growth, increased mitotic activity, and decreased cell low or high grade for dysplasia positive. In addition to the fact that it can be indefnite dysplasia in which dysplasia and regenerative/reac seen in benign lesions, it is a feature of real neoplastic epithe tive atypical changes can not be diferentiated are immediately lium, such as dysplasia or cancer. The answer to the Atypia is in 3 main types: question about whether it is real dysplasia or regenerative/re active hyperplasia is one of the most important problems of 1. The increase of the expression and its discontinuity such as acute infammation or radiation. Precancerous atypia (dysplasia/intraepithelial neoplasia): It methods in dysplasia diagnosis (21). However, in most of the develops as a neoplastic process without relation to reac studies, it is seen that molecular markers are limited in distin tive or regenerative causes, and it is a change of epithelium guishing the atypical hyperplastic lesions from low-grade dys that has a risk of developing cancer. The second important point in endoscopic biop sies after the diagnosis of dysplasia is made is correct grading, In addition to the aforementioned cytologic features of atypia, because the biological meanings and treatment approaches of there are also structural deformations, such as nuclear polar low and high-grade dysplasia are very diferent to each other. The support of im intestinal metaplasia of the glandular area, it should be evalu munohistochemical and other molecular methods is limited. With the replacement of native glands by epithelia-show Mild: 1%-30% ing metaplasia-atrophy related to metaplasia Medium: 31%-60% Severe: 61%-70% (the cystic dilatation of the gland is together 2. The decrease of the density of native glands and character with the epithelial atypia and intestinal metaplasia); 16 times ized by the increase in interglandular extracellular matrix increased risk of malignancy.
Cheap stendra 50mg on line
Patients with scoliosis have an inverse relation ing medications vs grapefruit purchase on line stendra, and abnormal pulmonary function. Patients with ship between the severity of scoliotic deformity and the obesity-hypertension syndrome often have pulmonary compliance of the thoracic cage. Most often they have basilar atelecta Ankylosing spondylitis limits rib cage expansion, and sis, low tidal volumes, and mild hypoxemia. If diaphragmatic patients tend to breathe primarily by diaphragmatic move excursion is severely limited, these patients may develop ment as the thoracic cage becomes increasingly immobile. The underlying condition may contribute tothe contribution of thoracic cage expansion to tidal breath additional problems. For example, patients with liver disease, ing falls as minute ventilation increases. The position of the ascites, or tumors also may have pleural effusions, further thoracic cage at end expiration often becomes fixed at a vol compromising lung function. The chest wall therefore trauma may be unable or unwilling to take deep inspirations exerts a greater than normal outward pull on the lungs, result because of pain. The flail is the paradoxical inward movement of the ventilation-perfusion maldistribution contributing to chest wall during inspiration, making ventilation inefficient hypoxemia and hypercapnia. Chest pain and diaphragmatic excursion, this finding has been attributed underlying lung contusions contribute to respiratory failure. Patients 2 burden on the chest wall and the diaphragm during inspira with ascites and abdominal tumors would be expected to be tion. In scoliosis and spondylitis, regional differences in the chest wall and diaphragm to be more inward than nor ventilation can be explained by differences in expansion mal. Thus the amount of gas that can be further expired from owing to local chest wall stiffness in spondylitis or asymmet the end-expiratory position (expiratory reserve volume ric deformity in scoliosis. The work of breathing is increased, especially when For reasons that are not clear, cor pulmonale is seen more minute ventilation increases. The larger mass of the chest often in chronic respiratory failure from scoliosis, sometimes wall and abdominal wall must be accelerated at each breath, in the absence of severe gas-exchange abnormalities; it may and additional energy is expended to move them during tidal be related to anatomic deformity or arrested development of breathing. It is likely that Clinical Features obesity associated with more peripheral distribution of added adipose tissue (eg, buttocks and extremities) has less Some patients with thoracic wall abnormalities have chronic effect on respiratory function, but this has not been studied. The due to further abrupt worsening of the chest wall disease, chronicity of respiratory failure can be confirmed by finding development of a lung complication such as pneumonia or an elevated plasma bicarbonate level. Patients present usually with rapid, liosis and increases with increasing scoliosis. As many as 50% shallow tidal breathing unless there is a disorder of ventila of patients with an angle greater than 80 degrees may be con tory control suggesting central hypoventilation. An angle of 100 degrees examination can show obvious chest wall deformity or seems to be associated with dyspnea on exertion and an angle decreased range of motion of the chest wall or diaphragm, greater than 120 degrees with alveolar hypoventilation. Wheezing, rhonchi, or stridor may Treatment be evidence of superimposed obstructive airway disease such as asthma, but kinking of large central and upper airways in Care of the patient with respiratory failure from thoracic wall scoliosis may be the cause. There is considerable tions such as pneumonia, left-sided heart failure, atelectasis, reported success with noninvasive positive-pressure ventila and pleural effusions. Lung persist, likely because of improvements in respiratory muscle volumes do not decrease routinely in proportion to excess function and improved respiratory gas exchange. Mechanical weight, and no marker of obesity such as weight/height2 ventilation is initiated if the patient requires additional ven (body mass index) predicts respiratory failure. For example, tilatory support to overcome increased metabolic require in otherwise normal subjects who are more than 160% of ments or during an acute exacerbation owing to infection or ideal weight, lung volumes and flows are usually found to be surgery. Such normal lung function may not persist, how to respiratory failure, patients often will respond after several ever, as these patients age, and the decline in lung function days of correction of hypoxemia and respiratory acidosis by with advancing age may be accelerated compared with demonstrating greatly improved respiratory drive. In addition, obesity is associated with Respiratory stimulant drugs such as progesterone and hypertension and cardiovascular disease, which themselves almitrine are not helpful. Central matic excursion are approached according to the type of hypoventilation in obesity (obesity-hypoventilation syn problem. Those with severe ascites may benefit from large drome) further dissociates the degree of obesity from the volume paracentesis or other efforts to decrease the volume severity of hypercapnia, as does the high prevalence of basi of ascites. Pain management is critical in patients following lar atelectasis causing hypoxemia. Patients with ascites from liver disease and pregnancy fre Treatment of flail chest depends on the severity of injury. The severity of respiratory impairment ratory failure develops, mechanical ventilation may be neces from decreased diaphragmatic excursion is highly unpre sary until chest wall mechanics recover. Only in rare cases is dictable, but most of the patients have some degree of hypox surgical repair indicated, including prolonged recovery, emia and only rarely develop hypercapnia. As the disorder progresses, sitive to preload reduction and rapid decrease of intravascu work of breathing increases. Other patients will respond with improved gas those without chronic respiratory failure. Although precipi exchange after a short period of supplemental oxygen or tated most often by exacerbation of airway obstruction from mechanical ventilation. While there is little chance of improv infection and increased sputum production, an important ing the underlying pathophysiology in severe scoliosis or factor leading to acute respiratory failure is inspiratory mus severe ankylosing spondylitis, weight reduction and treatment cle fatigue. During expiration, decreased lung elastic recoil lowers the distending pressure holding the Chronic Obstructive Pulmonary Disease airways open and leads to increased airway resistance. The mechanism of lung Increased dyspnea and cough; decreased exercise parenchymal destruction in the majority is unknown. Many patients volume, increased sputum purulence, and/or worsen with emphysema have clinical features of chronic bronchitis. Bacterial infection also may fol General Considerations low viral or Mycoplasma infection. When the increased force needed exceeds the capacity about whether the type and number of bacteria change sig of the inspiratory muscles, muscle fatigue ensues, and acute nificantly during an exacerbation. A recent study indicates respiratory failure results from inability to maintain minute that bacterial subtypes change during exacerbations even ventilation. Malnutrition, corticosteroids, hypophos though the same species are present chronically and during phatemia, hypokalemia, and other factors predispose exacerbation. Since bacteria quantity and quality are only patients to respiratory muscle fatigue. The number of inflammatory cells have maldistribution of ventilation and perfusion even when and the amount of other sputum components change during stable, and gas exchange worsens during acute exacerbations acute exacerbation. Hypoxemia generally is responsive to oxygen ther and more adherent to mucosal surfaces. Vagal efferent depresses central chemoreceptor-mediated ventilatory fibers in the vagus nerve stimulate increased airway smooth drive. Hypoxic stimulation of the carotid bodies is relatively muscle contraction and increased airway resistance. Several studies have shown that breathing pattern and the distribution of ventilation becomes more nonuni and minute ventilation do not change appreciably after form.
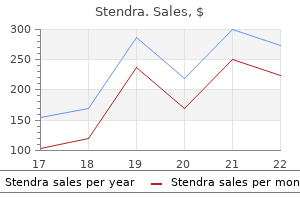
Purchase generic stendra canada
A General Considerations Aspiration pneumonia results from endotracheal aspiration of oropharyngeal or gastric secretions medicine wheel native american cheap 100 mg stendra with mastercard. Aspiration is thought to be a common occurrence in the healthy adult, with the incidence during sleep estimated to be as high as 45%. Small-volume aspirates are cleared by physical entrapment and coughing along with the mucociliary elevator action of the respiratory epithelium. Inactivation by IgA antibodies and opsonization and ingestion of bacteria by phagocytic cells play a role as well. Although organisms are present in pathogenic numbers even in small-volume aspirates, nor mal individuals are able to clear these organisms without sequelae. More caudally, dense consolidation with air bron with both high-volume, low-pressure cuffs and uncuffed or chograms secondary to pneumonia is present in the left low-volume, high-pressure tubes implicated. The consolidated lung enhances with contrast and of aspiration is even higher in patients with tracheostomies is easily distinguished from the surrounding pleural effusion. Nasogastric and feed ing tubes, gastric distention, gastroesophageal reflux, hiatal hernia, decreased esophageal mobility, and vomiting have all been cited as predisposing factors for aspiration. Bacterial colonization of gastric secretions also plays a role in intravenous contrast material facilitates differentiation of the development of aspiration pneumonia. Although gastric pleural and parenchymal disease because the lung acidity prevents significant bacterial colonization, antacid parenchyma will enhance with contrast, whereas the pleural therapy for prophylaxis for stress ulcers may change gastric effusion will retain its low attenuation. Aerobic bacteria associated with community acquired aspiration pneumonia are mostly streptococci, whereas gram-negative organisms, particularly Klebsiella and Escherichia coli, are seen more often in nosocomial infection. The major anaerobic organisms include Fusobacterium nucleatum, Peptostreptococcus, Bacteroides melaninogenicus, and Bacteroides intermedius. Atelectasis may be a feature of airway Aspiration pneumonia results in consolidation in dependent obstruction with food particles. The location of the consolidation will Franquet T et al: Aspiration diseases: Findings, pitfalls, and differen vary according to the patients position at the time of aspira tial diagnosis. Complications of simple aspiration pneumonia include General Considerations necrotizing pneumonitis and lung abscess. Lung abscess radiographically appears Emphysema and chronic bronchitis are the most com as a cavitary lesion within a focus of consolidation, usually mon examples. Four principal types of emphysema are described: centrilobular, panlobular, paraseptal, and paracicatricial. Chronic bronchitis is usually defined in clinical terms, manifested by chronic productive cough for at least 3 months for a minimum of 2 consecutive years and characterized by excessive secretion of mucus in the bronchi. Radiographic Features There is considerable controversy regarding the utility of the chest radiograph in the evaluation of emphysema. Although moderate to severe emphysema is usually apparent on the chest radiograph, mild disease is difficult to appreciate. Hyperinflation results from obstruction of small airways, resulting in air trapping. Bullae are recognized as hyperlucent or avascular regions and occasionally are demar cated peripherally by a fine curvilinear wall. The lung adja cent to large bullae may be compressed, and redistribution of pulmonary blood flow away from areas of extensive bullous disease may occur. The arterial deficiency pattern refers to regions of radiolucent, hypovascular pulmonary parenchyma characterized by a decrease in the size and num ber of vessels. Emphysema eventually can lead to pulmonary arterial hypertension, manifested radiographically by disproportion ate enlargement of the central pulmonary arteries and right heart chambers. The radiographic appearance of the lungs in chronic bronchitis is even less specific. Unlike that of emphysema, the diagnosis of chronic bronchitis is based on clinical symp toms and not morphologic appearance. In addition, chronic B bronchitis and emphysema frequently coexist, making pure chronic bronchitis difficult to characterize. Hyperinflation and hypovascularity have been ters, flattening of the diaphragm, and increased retroster described but are probably due to concomitant emphysema. Bowing of the upper zone in distribution and panlobular emphysema more sternum, another sign of hyperinflation, is seen more fre diffuse or more severe within the lower lobes. Bronchial wall thickening and cen for asthma and occurs in other pulmonary diseases associated trilobular abnormalities have been described. Exacerbation of asthma secondary to pneumonia is usually secondary to viral Hyperinflation. Lobar atelectasis occurs more often in children, with an inci Subsegmental atelectasis. General Considerations this complication occurs primarily in children; the pre Asthma is a disease characterized by widespread narrowing sumed mechanism is an increase in intraalveolar pressure of the airways that fluctuates in severity over short periods of and subsequent alveolar rupture secondary to mucous plug time either spontaneously or following therapy. Hyperactivity of airways may be induced by a variety of stim Central dissection of air along the perivascular sheaths uli, and asthma is usually divided into two types: intrinsic results in pneumomediastinum and may eventuate in subcu and extrinsic. In aerated lung, hypertrophy, mucosal edema, mucous hypersecretion, and pulmonary interstitial emphysema is usually not identifiable, plugging of airways by thick, viscid mucus. The result is nar but the sequelae of pneumomediastinum and pneumotho rowing of the airway diameter. The radiographic manifestations of asthma vary from a normal Although the findings of hyperinflation, increased perihilar radiograph to hyperinflation, atelectasis, or barotrauma. Most investigators fore not unanimously considered abnormalities and (2) find agree that a chest radiograph should be obtained when asthma ings that influence patient management. The incidence of is diagnosed initially to rule out other causes of wheezing such radiographic abnormalities depends on the age of the patient as airway obstruction by tumor or foreign body, congestive and the definition of abnormal by the investigator. In the patient with obvi may be seen with mucous plugging of small centrilobular ous (classic) epiglottitis, roentenographic diagnosis is not nec bronchioles, resulting in a tree-in-bud appearance. Sung A et al:the role of chest radiography and computed tomog Radiography may be useful in distinguishing epiglottitis raphy in the diagnosis and management of asthma. Chest radiograph usually abnormal but nonspecific, showing Ballooned hypopharynx, narrowed tracheal air column, atelectasis. Useful to exclude other causes of symptoms prevertebral soft tissue swelling, and obliteration of the such as pneumonia, pneumothorax, and pulmonary edema. Epiglottitis is a potentially lethal infection of the epiglottis and Ventilation-perfusion lung scan can be used to assess larynx resulting in supraglottic airway obstruction. In the pediatric patient, the causative of thrombus and parenchymal and pleural changes sec organism is usually Haemophilus influenzae, whereas in adults ondary to pulmonary embolism. Epiglottitis results for the diagnosis of pulmonary embolism, but is rarely in edema of the epiglottis, aryepiglottic folds, false cords, and performed. If clinical suspicion of pulmonary embolism is subglottic region and may involve the entire pharyngeal wall. However, sud General Considerations den death from airway obstruction is known to occur, and patients should be accompanied by a physician during the Pulmonary embolism is a common life-threatening disorder examination in the event that emergency endotracheal intuba that results from venous thrombosis, usually arising in the tion or tracheostomy is necessary. Radiographically, they appear as pulmonary embolism are nonspecific, and can be seen in a regions of parenchymal opacity adjacent to the pleura, typi variety of pulmonary and cardiovascular diseases.

Generic stendra 100 mg otc
The presence of neck stiffness and/or impaired conscious level indicates the need for urgent investigation medicine naproxen stendra 50 mg lowest price. Although intracranial tumours are uncommon in childhood, when they occur they tend to lie in the midline. As a result, obstructive hydrocephalus often develops acutely with headache as a prominent initial symptom. Characteristics: Diffuse, dull, aching, band-like headache, worse on touching the scalp and aggravated by noise; associated with tension but not with other physical symptoms. Attempt to reduce psychological stress and analgesic over-use (see medication-overuse headache). Two recognisable forms exist: Specific diagnostic criteria are required for migraine with and without aura. The headache has throbbing, unilateral, worsened by bright similar features, but it is often poorly light, relieved by sleep, associated with localised and its description may merge nausea and, occasionally, vomiting. The visual forms comprise: flashing lights, zig zags (fortifications), scintillating scotoma (central vision) and may precede visual field defects. The headache is recurrent, lasting from 2 to 48 hours and rarely occurring more frequently than twice weekly. Specific types of migraine with aura Basilar: Characterised by bilateral visual symptoms, unsteadiness, dysarthria, vertigo, limb paraesthesia, even tetraparesis. Hemiplegic: Characterised by an aura of unilateral paralysis (hemiplegia) which unusually persist for some days after the headache has settled. Retinal Unilateral (monocular) visual loss which is reversible and followed by headache. If vomiting is prominent anti-emetic (domperidone or prochlorperazine) and analgesic can be helpful. Medication Overuse Headaches Some patients with episodic tension headache or migraine find their headache pattern changes so that they have headaches most days. These do not respond to prophylactic agents and will improve on stopping the regular analgesics; this can take some weeks and headaches can be worse in the short-term. Transformed migraine If patients with migraine go on to develop chronic daily headache without overusing medication this is transformed migraine. Charecterised by episodes of severe unilateral pain, lasting 10 minutes to 2 hours, around one eye, associated with conjunctival injection, lacrimation, rhinorrhea and occasionally a transient Horners syndrome. The episodes occur between once and many times per day, often wakening from sleep at night. Other rarer combinations of facial pain and antonomic symptoms include: Hemicrania continua: continuous unilateral moderately severe head pain with exacerbations and variable tearing and partial Horners syndrome. The involved vessel, usually the superficial temporal artery, may be tender, thickened, and but nonpulsatile. Jaw claudication: pain when chewing or talking due to ischaemia of the masseter muscles is pathognomonic. Mechanism: Large and medium-sized arteries undergo intense giant cell infiltration, with fragmentation of the lamina and narrowing of the lumen, resulting in distal ischaemia as well as stimulating pain sensitive fibres. Blood film shows anaemia or Thickened wall with giant cell infiltrate thrombocytosis. Treatment: Urgent treatment, prednisolone 60 mg daily, prevents visual loss or brain-stem stroke, as well as relieving the headache. Most patients eventually come off steroids; 25% require long-term treatment and if so, complications commonly occur. Consider sudden severe headaches to be due to subarachnoid haemorrhage until proved otherwise. Systemic causes: Headache may accompany any febrile illness or may be the presenting feature of accelerated hypertension or metabolic disease. With ischaemic damage, as cell metabolism fails, intracellular Na+ and Ca2+ increase and the cells swell i. Various regulatory mechanisms acting on the arterioles maintain a cerebral blood flow sufficient to meet the metabolic demands. To meet such needs in the white matter, flow is 20 ml/100 g/min, whereas in the grey matter flow is as high as 100ml/100g/min. Neurogenic influences appear to have little direct effect on the cerebral vessels but they may alter the range of pressure changes over which autoregulation acts. As an intracranial mass expands and as the compensatory reserves diminish, transient pressure elevations (pressure waves) are superimposed. Eventually the rise in intracranial pressure and resultant fall in cerebral perfusion pressure reach a critical level and a significant reduction in cerebral blood flow occurs. When intracranial pressure reaches the mean arterial blood pressure, cerebral blood flow ceases. Inter-relationships are complex and feedback pathways may merely serve to compound the brain damage. Clinical effects the cerebral hemispheres results in a are difficult to distinguish vertical displacement of the midbrain from effects of direct and diencephalon through the tentorial brain stem/midbrain hiatus. Unchecked lateral tentorial herniation leads to central tentorial and tonsillar herniation, associated with progressive brain stem dysfunction from midbrain to medulla. They are often absent; when present they are invariably preceded by a deterioration in conscious level. In some patients, despite the above measures, cerebral swelling may produce a marked increase in intracranial pressure. This may follow removal of a tumour or haematoma or may complicate a diffuse head injury. Artificial methods of lowering intracranial pressure may prevent brain damage and death from brain shift, but some methods lead to reduced cerebral blood flow, which in itself may cause brain damage (see page 84). Intracranial pressure is monitored with a ventricular catheter or surface pressure recording device (see page 52). This method buys time prior to craniotomy in a patient deteriorating from a mass lesion. Repeated infusions, however, lead to equilibration and a high intracellular osmotic pressure, thus counteracting further treatment. In addition, repeated doses may precipitate lethal rises in arterial blood pressure and acute tubular necrosis. Sedatives: If intracranial pressure fails to respond to standard measures then sedation may help under carefully controlled conditions. Propofol, a short acting anaesthetic agent, reduces intracranial pressure but causes systemic vasodilatation. If this occurs pressor agents may be required to prevent a fall in blood pressure and a reduction in cerebral perfusion. Avoid high doses of Propofol; rhabdomyolysis may result and carries a 70% mortality. Barbiturates (thiopentone) reduce neuronal activity and depress cerebral metabolism; a fall in energy requirements theoretically protects ischaemic areas. Associated vasoconstriction can reduce cerebral blood volume and intracranial pressure but systemic hypotension and myocardial depression also occur. Clinical trials of barbiturate therapy have not demonstrated any improvement in outcome. Although this reduces intracranial pressure, the resultant reduction in cerebral blood flow may aggravate ischaemic brain damage and do more harm than good (see page 232).

Stendra 100 mg overnight delivery
Com plex tasks treatment 4 pimples order stendra with visa, prolonged, repetitive, and boring tasks were particularly sensitive to sleep deprivation. Similarly, tasks which involved short term memory, newly learned skills, and those skills not well practiced, were vulnerable to sleep deprivation, though self-paced tasks and feedback on perfor mance levels were able to reduce the effect. It appears that, for some less specific skills, even shorter periods of sleep loss may impair performance. Scanning ability may be reduced, suscep tibility to disorientation may be increased, and the ability to read charts may be affected. Pro bably most importantly, impairment of interpersonal skills and mood may result in failure of command, control, and crew coordination. Although the adverse effects of total absence of sleep extending beyond 24 hours are well recognized, impairment related to less severe degrees of sleep loss or irregularity of sleep are equally important. The most likely sleep problems encountered by aircrews in sustained opera tions are fragmented sleep associated with partial sleep loss, disruption of sleep wakefulness cycles and circadian rhythm disruption. For some individuals, the loss of only two and a half hours of sleep each night for two nights has been shown to impair vigilance the next morning, and so it must be suspected that repeated partial sleep loss will lead to impaired performance after several days of irregular work and rest. In addition, irregularity of sleep and the disruption of the normal sleep-wakefulness cycles, rather than a reduction of total hours of sleep, is also likely to 19-5 U. The factors which influence performance with total sleep loss are probably equally relevant to those which occur with partial sleep loss or disturbed sleep due to irregularity of work and rest. In conclusion, the effects of disturbed sleep (total absence, partial loss or irregularity) will con tinue to be a dominant issue in sustained air operations. Sleep is essential to sustain high levels of vigilance and maintain effectiveness. Careful attention to sleep is all important because impaired performance follows sleep disturbance even though impairment may not be easy to demonstrate. Circadian Desynchronosis Some studies suggest that the fragmentation of sleep and circadian desynchronosis (changes in circadian rhythm patterns and their interrelationships in man) have more importance than lost sleep on subjective mood or objective performance changes. Others feel that it is sleep depriva tion and not necessarily circadian desynchronosis which is the more important factor. For the flight surgeon concerned with operational fatigue, sleep deprivation and desynchronosis may be considered as being so entwined that each is essentially inextricable from the other. In recent years, a large body of information has accumulated showing time of day effects in performance, ranging from simple observations of performance at different times in the normal working day, to complex studies of work-rest schedules over prolonged periods. As a result of these studies, circadian rhythms in task performance, as well as subjective ratings of mood, fatigue, and motivation have been well established. Circadian desynchronosis will adversely influence performance in operations which require vigilance at times when the aircrew is usually asleep. Body temperature as well as the scores on most performance tests decline to a minimum between 0300 and 0600 hours and rise to a max imum during the day between 1200 and 2100 hours. It has been shown however, that there is no direct cause and effect relationship between body temperature and performance level. The range of oscillation in performance degradation during sustained operations depends on the phase of the circadian cycle it coincides with. When the operation commences during the beginning of a peak in the circadian cycle, the effect of fatigue is compensated in part by the increasing level of arousal during the day; when the operation commences during a period of decline in the circadian cycle, then the fatigue adds to the depression of alertness naturally occurring at night. Circadian desynchronization can occur in other ways than when a mission has to be flown dur ing the hours normally reserved for sleep. When an abrupt phase shift in the environmental tim ing system occurs, such as during rapid transmeridian flights, there is a transitory desynchroniza tion of the individuals circadian rhythmicity. This scenario is frequently seen in aircrew involved 19-6 Fatigue in world-wide operations. Another scenario involves fighter and attack aircraft which normally fly multiple short-duration missions separated by periods of nonflying activity. If this sequence continues around the clock, as in the case in some sustained carrier-based flight operations, then rhythm disturbances similar to those caused by rapid transmeridian dislocations may occur. Finally, when changes occur in environmental cues or these cues become weakened or disappear completely, as occurs in space operations, arctic living, or confinement to a shelter, circadian desynchronization may occur. In summary, fatigue, sleep loss, and circadian desynchronosis are so operationally entwined that a flight surgeon may consider them essentially inextricable from each other. The cumulative effects of sleep deprivation combined with circadian rhythm disturbances will result in impaired performance during sustained operations. Identifying Signs of Performance Decrement Identifying signs of an individuals performance degradation is a crucial first step in the management of fatigue and sleep loss involved in sustained flight operations. Mood and Motivational Changes Early symptoms of fatigue and insufficient sleep include less positive and more negative moods. Individuals may report feeling less willing to work due to lack of energy or feeling less alert, more irritable, and increasingly negative and sleepy. Individuals who regard sleepiness and mood changes as signs of weakness often deny negative moods and tiredness but may admit to decreased positive mood. Interesting tasks with relatively simple motor skills are resistant for periods as long as 60 hours, but routine monotonous tasks show a rapid decrement after 18 hours without sleep. Decreased initiative and increased negativism and irritability may lead to a decreased willingness to report events and to interact with other aircrew. Impaired Attention Fatigued and sleep deprived individuals have a shortened attention span and cannot concen trate on specific tasks with the same vigilance and sustained alertness as when they are rested. In termittent dream-like intrusions or irrelevant thoughts cause lapses of attention and decreased ability to concentrate. As fatigue and sleep deficit progress, the duration and number of lapses of attention increase. Memory Loss for Recent Events A well-recognized sign of sleep loss is the ability to recall what you just heard, saw, or read. An individual who is fatigued and sleep deprived may remain confident about retaining messages, data, and events only to realize later that these have been forgotten. Loss of sleep for 24 hours impairs the acquisition of infor mation and newly retained material. After 48 hours of continuous work there is a drop below 40 percent of baseline levels of performance on tests that require recent memory. Variable and Slowed Responses During continuous work episodes speed and accuracy suffer. Speed is most often decreased in order to maintain accuracy, not necessarily as a slowing down of all responses, but more as an unevenness in response time. The danger of fatigue and sleep loss is the unpredictable slowing down of appropriate responses. Depending upon the task, some situations are more sensitive to sleep loss and fatigue than others, and the longer the tasks, the more obvious are the changes. The loss of one nights sleep may have little effect during the first five minutes of a vigilance task, but when the task is extended to 15 minutes, performance deteriorates. Total sleep loss after 50 hours impairs responses after three minutes and after 70 hours responses are impaired within only two minutes. Increasing the dif ficulty of the task causes variable and slowed responses to be even more sensitive to performance decrement. When an addition task is required every two seconds no change can be detected even after two nights sleep loss, but when the speed of addition is increased to one problems every 1. Lack of Insight on Impaired Performance Deficits associated with continuous work episodes may be underestimated and disregarded. In dividuals may be more easily satisfied with lower levels of performance and errors may be recognized but not corrected. Decrements in performance on a primary task can be avoided, but secondary tasks, incorrectly thought to be less critical, are impaired. In addition, the individual may lose flexibility of approach and the ability to perceive or adjust to new aspects of a problem. Impaired Task Performance As sleep deprivation continues, the individuals performance may continue on a reasonable level of efficiency but will be broken by lapses of attention. Sleep deprived subjects may carry out tasks accurately, but their periods of accuracy become briefer and more infrequent as the depriva 19-8 Fatigue tion continues. Performance decrement is seen as brief intermittent lapses in performance which increase in frequency and duration.
Pinus larix (Larch Arabinogalactan). Stendra.
- What is Larch Arabinogalactan?
- Common cold, flu, liver disease, high cholesterol, earache (otitis media), HIV/AIDS, cancer treatment, dietary fiber supplementation, stimulating the immune system, inflammation, and other conditions.
- How does Larch Arabinogalactan work?
- Are there any interactions with medications?
- Are there safety concerns?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96935
Discount stendra 50mg with amex
Ask about smoking medicine lodge kansas cheap 200mg stendra, tobacco chewing, alcohol use, fe ver, pain, weight loss, night sweats, exposure to tuberculosis, animals, pets, and occupational/sexual history. Physical Exam All mucosal surfaces of the nasopharynx, oropharynx, larynx, and nasal cavity should be visualized by direct examination or by indirect mirror or fiberoptic visualization. Regarding the neck mass, emphasis on location, tenderness, mobility, and consistency of the neck mass can often place the mass within a general etiologic grouping. Criteria such as heterogeneity of the center of the mass, blurred borders, and a round shape are suggestive of malignancy. Contrast should be used except in the suspected thyroid lesion as it may interfere with radioactive-iodine imaging studies or therapy. M R I i s c o m p a r a b l e t o C T, b u t i t i s m o r e e x p e n s i v e a n d h a s l o n g e r i m a g i n g time. Ultrasound is helpful in differentiating solid from cystic masses and con genital cysts from solid lymph nodes and glandular tumors. Labs A r o u t i n e c o m p l e t e b l o o d c o u n t t e s t m a y r e v e a l a n i n f e c t i o u s p r o c e s s. M o r e s p e cialized laboratory tests may become necessary as the investigation proceeds. G Panendoscopy: If careful examination in the office does not identify the etiology of the neck mass and a tumor is suspected, the upper aerodi gestive tract should be examined under anesthesia. N Treatment Options Medical A t e n d e r, m o b i l e m a s s o r o n e h i g h l y s u g g e s t i v e o f i n f l a m m a t o r y o r i n f e c t i o u s etiology may warrant a short clinical trial of antibiotics and observation with close follow-up. Use steroids judiciously; steroids may shrink a neck mass caused by lymphoma lulling the physician and patient into a false sense that the condition is improving. Surgical G Open excisional biopsies should be avoided in cases in which a nonlym phoma malignancy (epidermoid, melanoma) is suspected. The patient and surgeon should be prepared to proceed immediately with a complete neck dissection depending on the results of frozen sections. G Open excisional biopsies may be performed for lymphomas or granu lomatous disease. G Inflamed congenital masses are typically treated with antibiotics and then surgically removed after inflammation has subsided. Surgery in the form of incision and drainage is used in cases that do not respond to appropriate medical therapy. Squamous cell carcinoma metastatic to the neck from an unknown head and neck primary site. Am J Otolaryngol 2001;22(4):261267 346 Handbook of OtolaryngologyHead and Neck Surgery 5. G There is a propensity for second primary tumors (between 4 and 7% per year), especially if still smoking. Specific sites and subsites of head and neck cancer are discussed in subsequent chapters. These cancers are more common in men, and typically occur in patients over age 50. The etiology includes tobacco use (smoking and smokeless) and alcohol consumption. The synergistic effect of alcohol and smoking increases the risk of disease many more times than the simple additive risk of either risk factor alone. Head and Neck 347 N Clinical Signs Signs may include hoarseness, muffled speech, trismus, and recurrent epistaxis. Many patients present with a neck mass as chief complaint, representing metastatic nodal disease from an occult primary tumor in the upper aerodigestive tract (Table 5. Early symptoms may be vague and mimic benign disease and are therefore only discovered at advanced stages of disease. Differential Diagnosis G Upper respiratory infections such as pharyngitis, laryngitis, deep neck infections or abscesses G Congenital masses and cysts G Upper airway manifestations of rheumatologic and autoimmune diseases G Hematologic malignancies (lymphoma) G Tuberculosis G Fungal infections Table 5. Physical Exam Physical exam should include careful inspection of the oral and oropharyn geal mucosa for lesions, and palpation of the tonsillar region and tongue base for firm nodules or masses. During this examination, the patient should be asked to perform several maneuvers such as tongue protrusion, puffing out the cheeks, lightly coughing and speaking to better visualize and access the larynx and the hypopharynx. Any palpable lymph nodes should be assessed with regard to size, location, and mobility. Specific characteristics of regional lymphadenopathy, if present, should be noted, such as extracapsular spread, central necrosis, and size of involved lymph nodes. Labs Blood count, electrolyte, and liver function tests should be performed to assess nutritional status. It is best to avoid open bi opsy of a neck mass, as tumor spillage and violation of fascial planes is problematic. Head and Neck 349 laryngoscopy, esophagoscopy, and bronchoscopy together, to search for synchronous lesions. This may also lend insight as to the extent of the primary lesion, particularly important in the smoking patient. Surgical resection remains the gold standard for treatment of head and neck cancer. Individual chemotherapeutic agents effective in the therapy of head and neck cancer include cisplatin, methotrexate, 5-fluorouracil, taxanes, ifosfamide, and bleomycin. N Cancer of Unknown Primary Patients with head and neck cancer typically present with a painless neck mass. A primary tumor is considered unknown only after a thorough investigation (including physical exam, imaging, and biopsies) has been completed. The next step is to perform panendoscopy with biopsies whether or not the primary site was located on imaging. As noted earlier, panendoscopy typically included bronchoscopy, esophagoscopy, and direct laryngoscopy. If no obvious tumor is visualized, tonsillectomy and guided biopsies are performed. Some advocate a unilateral tonsillectomy limited to the side of the neck mass, but others advocate bilateral tonsillectomies in this circum stance. Each of these sites should at least be inspected with consideration of guided biopsies. Surgical excision in the form of a neck dissection followed by radiation therapy allows for a lower total dose of radiation. Primary radiation therapy provides treatment to both the upper aerodigestive tract and its locoregional metastasis but forces the radiation oncologist to treat a wider field as the primary site is unknown. This should include the surgical oncologist, medical and radiation oncologist, oral surgeon, prosthodontist, speech language and swallowing pathologist, nurse, and social worker. There is controversy as to the need for a planned neck dissection following radiotherapy in patients with high-risk disease. There is no evidence that routine follow-up beyond 3 years improves prognosis, although many clinicians support yearly follow-up. Patients should be told of the risk of a second primary tumor and encour aged to report any new symptoms. Head and Neck 351 N Staging of Head and Neck Cancer Gthe regional lymph node metastases and their effect on stage grouping are fairly consistent throughout all anatomic sites of head and neck cancer. N0 No evidence of regional lymph node metastasis N1 Metastasis to a single ipsilateral lymph node measuring #3 cm in greatest diameter N2 Further divided into three categories: N2a Single ipsilateral lymph node between 3 and 6 cm N2b Multiple ipsilateral lymph nodes $6 cm N2c Bilateral or contralateral lymph nodes $6 cm in greatest dimension N3 Lymph node "6 cm G Distant metastatic disease is divided into two categories: M0 Absence of distant disease M1 Presence of distant metastatic disease Gthe T stage of a tumor indicates the extent of the primary tumor and varies by anatomic subsite. This can be measured by size, as in the oral cavity, oropharynx, and salivary glands; by involvement of varying sub sites, as in the nasopharynx, hypopharynx, and larynx; or by extent of invasion and destruction, as in the maxillary sinus. Diagnostic evaluation of squamous cell carcinoma metastatic to cervical lymph nodes from an unknown head and neck primary site. Positron emission tomog raphy in the management of unknown primary head and neck carcinoma. Head Neck 2008;30(1):2834 352 Handbook of OtolaryngologyHead and Neck Surgery 5. G Palliative chemotherapy can reduce symptoms and modestly extend survival in an incurable setting. G Newer biologic and cytotoxic agents continue to cause the treat ment of head and neck cancer to evolve. The role of chemotherapy in head and neck cancer is expanding and its utility varies with the stage of the disease. For patients with metastatic or incurable locoregional disease, chemotherapy is palliative.
Syndromes
- Tall, thin build
- Worsening vision
- Surgical removal of burned skin (skin debridement)
- Disorders of the nerves that supply the intestines
- Severe low blood sugar (hypoglycemia)
- Blood clots
Order stendra 200 mg with visa
Log kill: Destruction of cancer cells by chemotherapeutic agents follows first-order kinetics; that is treatment 4 pink eye discount 200mg stendra overnight delivery, a given dose of drug destroys a constant fraction of cells. For 9 example, a diagnosis of leukemia is generally made when there are about 10 (total) leukemic cells. For most bacterial infections, a five-log (100,000-fold) reduction in the number of microorganisms results in a cure, because the immune system can destroy the remaining bacterial cells. However, tumor cells are not as readily eliminated, and additional treatment is required to totally eradicate the leukemic cell population. Therefore, a patient may require irradiation of the craniospinal axis or intrathecal administration of drugs to eliminate the leukemic cells at that site. Treatment protocols: Combination-drug chemotherapy is more successful than single-drug treatment in most of the cancers for which chemotherapy is effective. Combinations of drugs: Cytotoxic agents with qualitatively different toxicities, and with different molecular sites and mechanisms of action, are usually combined at full doses. In contrast, agents with similar dose-limiting toxicities, such as myelosuppression, nephrotoxicity, or cardiotoxicity can be combined safely only by reducing the doses of each. Advantages of drug combinations:the advantages of such drug combinations are that they 1) provide maximal cell killing within the range of tolerated toxicity, 2) are effective against a broader range of cell lines in the heterogeneous tumor population, and 3) may delay or prevent the development of resistant cell lines. Treatment protocols: Many cancer treatment protocols have been developed, and each one is applicable to a particular neoplastic state. Problems associated with chemotherapy Cancer drugs are toxins that present a lethal threat to the cells. It is therefore not surprising that cells have evolved elaborate defense mechanisms to protect themselves from chemical toxins, including chemotherapeutic agents. Resistance: Some neoplastic cells (for example, melanoma) are inherently resistant to most anticancer drugs. Other tumor types may acquire resistance to the cytotoxic effects of a medication by mutating, particularly after prolonged administration of suboptimal drug doses. The development of drug resistance is minimized by short-term, intensive, intermittent therapy with combinations of drugs. Drug combinations are also effective against a broader range of resistant cells in the tumor population. A variety of mechanisms are responsible for drug resistance, each of which is considered separately in the discussion of a particular drug. Multidrug resistance: Stepwise selection of an amplified gene that codes for a transmembrane protein (P-glycoprotein for apermeabilitya glycoprotein; Figure 39. This resistance is due to adenosine triphosphateadependent pumping of drugs out of the cell in the presence of P-glycoprotein. For example, cells that are resistant to the cytotoxic effects of the vinca alkaloids are also resistant to dactinomycin, to the anthracycline antibiotics, as well as to colchicine, and vice versa. These drugs are all naturally occurring substances, each of which has a hydrophobic aromatic ring and a positive charge at neutral pH. It has been suggested that the presence of P-glycoprotein may account for the intrinsic resistance to chemotherapy observed with adenocarcinomas. However, these drugs are undesirable because of adverse pharmacologic actions of their own. Common adverse effects: Most chemotherapeutic agents have a narrow therapeutic index. Severe vomiting, stomatitis, bone marrow suppression, and alopecia occur to a lesser or greater extent during therapy with all antineoplastic agents. Some toxicities, such as myelosuppression that predisposes to infection, are common to many chemotherapeutic agents 39. For example, alopecia is transient, but the cardiac, pulmonary, and bladder toxicities are irreversible. The megaloblastic anemia that occurs with methotrexate can be effectively counteracted by administering folinic acid (leucovorin, 5-formyltetrahydrofolic acid; see below). With the availability of human granulocyte colony-stimulating factor (filgrastim), the neutropenia associated with treatment of cancer by many drugs can be partially reversed. Treatment-induced tumors: Because most antineoplastic agents are mutagens, neoplasms (for example, acute nonlymphocytic leukemia) may arise 10 or more years after the original cancer was cured. Antimetabolites Antimetabolites are structurally related to normal compounds that exist within the cell. Their maximal cytotoxic effects are in S-phase (and, therefore, cell-cycle) specific. Methotrexatethe vitamin folic acid plays a central role in a variety of metabolic reactions involving the transfer of one-carbon 1 units and is essential for P. Mechanism of action: Folic acid is obtained from dietary sources or from that produced by intestinal flora. This inhibition deprives the cell of folate coenzymes and leads to decreased production of compounds that depend on these coenzymes for their biosynthesis. Although these molecules include the nucleotides adenine, guanine and thymidine and the amino acids methionine and serine, depletion of thymidine is the most prominent effect. Therefore, it is important to keep the urine alkaline and the patient well hydrated to avoid renal toxicity. Commonly observed toxicities: In addition to nausea, vomiting, and diarrhea, the most frequent toxicities occur in tissues that are constantly renewing. Some of these adverse effects can be prevented or reversed by administering leucovorin (see Figure 39. Occurrance of hepatotoxicity in the form of jaundice has been reported in about one-third of adult patients. This results in unexpectedly high myelosuppression and has also been associated with the occurrence of secondary malignancies. To a lesser extent, 6-thioxanthine and 6-thiouric acid are also formed by the action of guanase. It is useful in the treatment of chronic lymphocytic leukemia and may replace chlorambucil, the present drug of choice. Fludarabine is a prodrug, the phosphate being removed in the plasma to form 2-F-araA, which is taken up into cells and again phosphorylated (initially by deoxycytidine kinase). In addition to nausea, vomiting, and diarrhea, myelosuppression is the dose-limiting toxicity. At high doses, progressive encephalopathy, blindness, and death have been reported. Resistance may be due to mechanisms analogous to those that affect fludarabine, although cross-resistance is not a problem. Adjuvant therapy with levamisoleaa veterinary anthelmintic agentaimproves the survival of some patients with colon cancer. A dermopathy (erythematous desquamation of the palms and soles) called the ahand-foot syndromea is seen after extended infusions. It is approved for the treatment of metastatic breast cancer that is resistant to first-line drugs (for example, paclitaxel and anthracyclines) and is currently also used for treatment of colorectal cancer. This step is catalyzed by thymidine phosphorylaseaan enzyme that is concentrated primarily in tumors 39. Pharmacokinetics: Capecitabine has the advantage of being well absorbed following oral administration. Capecitabine should be used cautiously in patients with hepatic or renal impairment. Patients taking coumarin anticoagulants or phenytoin should be monitored for coagulation parameters and drug levels, respectively. The common adverse effects are nausea, vomiting, diarrhea, enteritis, stomatitis, and localized erythema. Pharmacokinetics: Ara-C is not effective when given orally, because of its deamination to the noncytotoxic uracil arabinoside (ara-U) by cytidine deaminase in the intestinal mucosa and liver. Ara-C undergoes extensive oxidative deamination in the body to ara-Uaa pharmacologically inactive metabolite. Adverse effects: Nausea, vomiting, diarrhea, and severe myelosuppression (primarily granulocytopenia) are the major toxicities associated with ara-C. At high doses or with intrathecal injection, ara-C may cause leukoencephalopathy or paralysis. It is used for the first-line treatment of locally advanced or metastatic adenocarcinoma of the pancreas. It also is effective against nonasmall cell lung cancer and several other tumors.
Purchase stendra 100 mg visa
A ing these complications k-9 medications discount stendra uk, with subsequent decreased perfusion repeat cross-match will demonstrate a new antibody. The degree of dam some exceptions, hemolysis is extravascular and mild, without age is related to the dose of incompatible blood received. Any transfusion complicated by even apparently mild No specific therapy is necessary, but if indicated clinically, fur findings such as fever or allergic symptoms should be ther transfusion should be given with red blood cells negative stopped. If the patient has never been record of the antibody, and all future red blood cell transfu transfused or has never had any adverse reaction to prior sions should be with antigen-negative blood. The patient transfusions, even a minor febrile reaction should prompt an should be informed of the antibody and of the need for screen evaluation for incompatibility. The remainder of the unit of ing of all future transfused red blood cells to avoid another such blood and additional samples (anticoagulated and coagu reaction. The patient also should be monitored for the develop lated) from the patient should be sent to the blood bank for ment of other antibodies following subsequent transfusions. If acute hemolysis has occurred, the patient should be Since there are over 300 red blood cell antigens, virtually all managed with aggressive supportive care. Vital signs should be red blood cell transfusions expose the recipient to foreign monitored and intravenous volume support provided to antigens. Most antigens are not immunogenic, however, and maintain adequate blood pressure and renal perfusion for at rarely result in development of alloantibodies. Loop or osmotic influence the development of alloantibodies include the diuretics may be used in combination with intravenous fluids immunogenicity of the antigen, the frequency of the antigen to maintain renal perfusion and urine output over 100 mL/h. It is response, alloantibodies do not complicate the sensitizing important to remember that an adverse reaction to an incom transfusion. Subsequent cross-match procedures will detect patible unit of red blood cells does not obviate the initial need most clinically significant alloantibodies, but the develop for the transfusion. Therefore, transfusion with compatible ment of multiple alloantibodies may make it difficult to find red blood cells should be undertaken to provide the oxygen compatible units for transfusion-dependent recipients. Delayed hemolytic transfusion reactions may occur if the In a patient who had been transfused previously and has antibody is not detectable at the time of subsequent cross had prior febrile reactions, the decision to evaluate each match procedures. Red blood cell phenotyping may be useful subsequent febrile reaction may be difficult. At a minimum, for transfusion-dependent patients who demonstrate a ten verification of the identity of the unit and the patient always dency for antibody formation. Whether to initiate the entire evalua in the frequency of antigens exist between donor and recip tion for hemolysis will depend on the clinical circumstances. Alternatively, if negative red blood cells for sickle cell patients) to prevent judged safe to continue without further evaluation, antipyret alloimmunization. Infection Clinical Significance/Incidence Viruses Hepatitis A Rarely transmitted because of short period of viremia and lack of carrier state (1 in 1,000,000 units transfused) Parvovirus B19 Estimated risk is 1 in 10,000 units transfused. Infection clinically insignificant except in pregnant women, patients with hemolytic anemia or who are immunocompromised. Cytomegalovirus Clinically significant transfusion complication in low-birth-weight neonates or immunocompromised hosts. Blood stored for more than 14 days and noncel lular components are not infectious. Twenty to forty percent of recipients receiving infected blood become infected with virus; infection may lead to T cell lymphoproliferative disorder or myelopathy after long latency period. Usually causes anicteric and asymptomatic hepatitis 6 weeks to 6 months after transfusion. Delta agent Cotransmitted with hepatitis B, found primarily in drug abusers or patients who have received multiple transfu sions. Superinfection of hepatitis B surface antigen carriers may result in fulminant hepatitis or chronic infectious state. Hepatitis C Previously the leading cause of posttransfusion hepatitis; donors are now screened, with estimated risk 1:600,000. Bacteria Environmental contaminants Closed, sterile collection techniques, use of preservatives and refrigeration, and natural bactericidal action of blood ensures extremely low risk, but improper storage or contamination with pathogens that survive refrigera tion may result in serious bacterial infection. Donor-transmitted Asymptomatic carriers of certain bacteria may transmit infection; Yersinia enterocolitica is most common (<1:1,000,000) and is highly fatal. Other organisms (salmonella, brucella) associated with chronic carrier state are transmitted less often. New standards to detect bacterial contamination of stored platelets should reduce this risk. Lyme disease Borrelia burgdorferi viable much longer than Treponema pallidum, but the period of blood culture positivity is associated with symptoms that preclude donation. Toxoplasmosis Infrequent hazard of granulocyte transfusion in immunosuppressed hosts. Screening includes obtaining historical infor gery, during initial treatment for hematologic malignancies, mation from potential donors to identify risk factors for following massive transfusion in organ recipients, and in infectious diseases and performing tests to identify carriers patients receiving plasma for warfarin reversal or thrombotic of known transmissible agents (see above) and those at high thrombocytopenic purpura. Characteristics of agents score the need for selecting patients appropriately for trans transmissible by blood include the ability to persist in blood fusion therapy. Perioperative Transfusion Nonhemolytic, Noninfectiousthe need for transfusion in the perioperative period should Complications be determined by individual patient characteristics and by Nonhemolytic, noninfectious transfusion reactions account the type of surgical procedure rather than by hemoglobin for more than 90% of adverse effects of transfusions and level alone. Chronic mild to moderate anemia does not occur in approximately 7% of recipients of blood compo increase perioperative morbidity and by itself is not an indi nents. Major features of these unwanted complications are cation for preoperative red blood cell transfusion. Complication Clinical Manifestations, Pathogenesis, Prevention, and Treatment Strategies Febrile-associated transfusion Occurs in 0. Urticaria, pruritus, bronchospasm, or frank anaphylaxis due to recipient sensitiza tion to a cellular or plasma element. Leukocyte depletion or washed red cells may be necessary for subsequent transfusions. Treat with oxygen, diuretics, and, rarely, phlebotomy (save units for reinfusion if necessary). Dilutional effects Transfusing with more than one blood volume or red blood cells with dilute platelets and coagulation factors. Hyperkalemia May occur in patients with preexisting renal insufficiency and hyperkalemia or in neonates. Use of fresh blood or washed red cells decreases potassium load for these patients. Hypothermia After massive transfusion of refrigerated blood, hypothermia may cause cardiac arrhythmias. Refrigerated blood may accelerate hemolysis in patients with cold agglutinin disease. Immune modulation Mechanisms and clinical significance unclear for immunosuppression that follows transfusion; enhances results following renal transplantation; possible deleterious effect on outcome after colorectal cancer surgery; possible increased susceptibility to bacterial infections. Prevent by irradiating all blood components with 2500 cGy for immunocompromised recipients or when donor is first-degree relative. Iron overload Multiple transfusions in the absence of blood loss lead to excess accumulation of body iron with cirrhosis, heart failure, and endocrine organ failure. Prevent by decreasing total amount of red cells given, using alternatives to red cells whenever possible, using neocytes, and modifying diet to decrease iron absorption. Iron chelation indi cated for patients with chronic transfusion dependence if prognosis is otherwise good. Posttransfusion purpura Acute severe thrombocytopenia about 1 week after transfusion due to alloantibodies to donor platelet antigen (usually P1A1). Self-limited, but treatment with steroids, high-dose IgG, plasmapheresis, or exchange transfu sion recommended to prevent central nervous system hemorrhage.
Cheap 200 mg stendra with mastercard
Less-severe initial loss treatment west nile virus generic stendra 50 mg amex, shorter duration of loss, and early treatment are associated with better recovery. Auditory rehabilitation in patients who fail to recover is important, especially in children. These range from injury to the auricle, the external ear canal, the tympanic mem brane, the ossicles, the inner ear, and the facial nerve. N Epidemiology Overall, between 14 and 22% of skull fractures involve the temporal bone. Traumatic tympanic membrane perforations have been estimated to occur at an annual incidence of 1. Lacerations, avulsions, hematomas, and thermal injuries to the auricle are common. Otology 105 N Clinical Signs and Symptoms Symptoms and signs depend on the type and extent of injury. Auricular Injury Blunt injury may result in local pain and swelling with auricular hematoma. Burns to the auricle may appear mild or full thickness; underlying cartilage viability is the critical concern. The auricle is a common site of frostbite injury, which may present as a spectrum of symptoms over several weeksfrom clear blistering, hemor rhagic blisters, a dry insensate wound, to blackened tissue demarcation. Penetrating Trauma or Perforations Foreign body, instrumentation, blunt injury, acoustic trauma, and barotrauma may all cause traumatic tympanic membrane rupture as well as middle or inner ear damage. Temporal Bone Fracture this is associated with severe traumatic head injury and the patient will present as such, requiring resuscitation, stabilization and multiteam care. Victims may present with Battles sign (mastoid bruise), raccoon eyes (periorbital bruising), otorrhea, hearing loss, nystagmus, and other cranial neuropathies. Differential Diagnosisthe differential diagnosis may include soft tissue injury, an auricular hematoma, a cartilage injury, a tympanic membrane perforation, an ossicular disruption, a perilymph fistula, an inner ear injury, a temporal bone fracture, and a facial nerve injury. In a trauma patient with severe head injury or multisystem injury, standard trauma protocol and resuscitation are performed. With severe injuries requiring intubation and other treatment, 106 Handbook of OtolaryngologyHead and Neck Surgery. In uncooperative children, there should be a low threshold for exam under anesthesia. Traumatic perforations may require surgical exploration if located in the posterosuperior quadrant and associated with severe vertigo. Soft tissue injuries isolated to the auricle are treated with focused exam and emergency care. Electrophysiologic testing of the facial nerve in the setting of traumatic paralysis may be helpful in terms of predicting recovery and guiding treatment decisions. N Treatment Options Soft Tissue Injuries Auricular lacerations must be cleaned thoroughly. If tissue is devitalized, wet-to-dry dressing coverage can be provided and surgical reconstruction planned in a delayed fashion. There is a high failure rate, requiring delayed debridement and discussion of reconstructive options. Most animal bites are thoroughly irrigated, closed, and treated with oral antibiotics. Penetrating Trauma/Perforations Ear canal lacerations should be suctioned and cleaned under the microscope. Traumatic perforations in the posterosuperior quadrant with symptom atic vertigo should undergo exploratory tympanotomy due to possible stapes dislocation. At surgery, unstable bone fragments are removed and the oval window is grafted; prosthesis placement is controversial. Antibiotic steroid drops are prescribed, dry ear precautions observed, nose blowing avoided, and follow-up exams planned. Large perforations or an accompanying infection may complicate healing and eventually require surgical repair. If there is complete facial nerve paralysis, this may require surgical exploration, depending on the nature of the injury. Gunshot wounds may involve widespread injury, carrying a high incidence of severe vascular injury and high mortality rate. Vestibular dysfunction is treated with rest and antiemetics; follow-up vestibular testing is performed. N Outcome and Follow-Up For temporal bone injuries involving hearing loss, follow-up audiograms are required, as discussed above. Most traumatic perforations heal spontaneously but should be reassessed at 3 months. Benign paroxysmal peripheral vertigo is common following temporal bone injuries, and is managed with canalith repositioning exercises. For patients without hearing recovery, auditory re habilitation options should be offered, ranging from a conventional hearing aid, a bone-anchored hearing aid, to possible cochlear implantation. Bell palsy, or acute idiopathic facial nerve palsy, accounts for 60 to 75% of all acute facial palsies. It is characterized by a rapid onset (24 to 48 hours), and may or may not progress to total paralysis. A facial weakness that progresses slowly over weeks to months is suspicious for a neoplasm. Treatment for Bell palsy consists of a prednisone taper (starting at 1 mg/kg) plus an antiviral for at least one week. If there is little to no recovery after 2 to 3 months, then imaging is recommended to rule out a neoplasm. N Epidemiologythe incidence of Bell palsy is 20 to 30 cases per 100,000 people per year. It accounts for almost 75% of all unilateral facial palsy; 40,000 cases occur in the United States each year. N Clinical Signs and Symptoms Patients usually present with rapid-onset (2448 hours) facial nerve weak ness that may progress to complete paralysis. Patients often report pain and numbness around the ear, hyperacusis, and dysgeusia; 70% of patients will have a preceding viral illness. Differential Diagnosis Idiopathic facial nerve palsy is a diagnosis of exclusion. Herpes zoster oticus (Ramsay-Hunt) is characterized by severe otalgia and vesicular lesions involving the ear, and accounts for 10 to 15% of acute facial palsies. Melkersson-Rosenthal syndrome consists of recurrent bouts of unilateral facial palsy in association with facial edema and a fissured tongue. Many advocate surgical decompression only for cases of complete paralysis, and, although not specifically indicated on this algorithm, facial nerve decompression may be useful in cases of nontraumatic paralysis. Acute and chronic otitis media with or without cholesteatoma can also cause acute facial palsy, as can necrotizing or malignant otitis externa. Neo plasms need to be ruled out if there is no symptomatic improvement after 2 to 3 months or if the palsy is characterized by slow onset or relapse. Total paralysis Complete paralysis Physical Exam A complete head and neck examination is required. The HouseBrackmann scale is often used for charting and physician communication (Table 2. The eardrum is carefully inspected to rule out acute or chronic middle ear disease, cholesteatoma, or a temporal bone neoplasm, either benign or malignant. They may be periauricular, auricular, in the ear canal, or even on the palate, and are expected to be tender and in various stages of healing. Palpation of the neck and parotid gland is crucial in ruling out an extratemporal process. The remaining cranial nerves are also examined looking for evidence for polyneuropathy. Imaging Imaging is not routinely obtained at presentation if the history is consistent with acute idiopathic palsy. If the palsy shows no signs of improve ment within 3 months, many clinicians will then order appropriate imaging as described. Some clinicians will not initially image patients with paresis, but then obtain imaging if the paresis progresses to complete paralysis. If the clinical picture does not follow that of an idiopathic palsy, or there are risk factors for other disorders then labs are ordered as indicated.